Anaplastic Large Cell Lymphoma, ALK-Positive
editPREVIOUS EDITIONThis page from the 4th edition of Haematolymphoid Tumours is being updated. See 5th edition Table of Contents.
Primary Authors*
Miguel Gonzalez Mancera, MD
Sumire Kitahara, MD
Cedars-Sinai, Los Angeles, CA
Cancer Category/Type
Cancer Sub-Classification / Subtype
- Systemic T-cell lymphoma
Definition / Description of Disease
Anaplastic Large Cell Lymphoma, ALK-Positive (ALK+ ALCL) is a T-cell lymphoma characterized by usually large lymphoma cells with abundant cytoplasm and pleomorphic nuclei, often horse-shoe shaped (see Morphologic Features below), with a chromosomal rearrangement involving the ALK gene resulting in expression of ALK protein and CD30
Synonyms / Terminology
- Ki-1 (CD30) lymphoma - obsolete
Epidemiology / Prevalence
- ALCL (ALK+, ALK-, and primary cutaneous) account for <5% of all cases of non-Hodgkin lymphoma (NHL)[1]
- ALK+ ALCL[1]
- ~3% of adult NHL
- 10-20% of childhood lymphomas
- Most frequent in the first three decades of life
- Male:female = 1.5:1
Clinical Features
- Most patients (70%) present with advanced (stage III-IV) disease and B-symptoms.[2]
Sites of Involvement[1]
- Lymph nodes and extranodal sites (most commonly skin, bone, soft tissue, lungs and liver)
- Bone marrow involvement detected in 30% when using immunohistochemistry (CD30 and EMA). Can miss marrow involvement by H&E evaluation alone, which detects involvement with ~10% incidence.[3]
Morphologic Features
- Lymphoma cells characterized by eccentric, horseshoe-shaped or kidney-shaped nuclei, often with eosinophilic cytoplasm accentuated near the nucleus
- Usually large in size, but may also be smaller
- Present in varying proportions
- Seen in all morphological variants/patterns of ALK+ ALCL
Morphological variants/patterns
- Common (60%): predominant population of large hallmark cells
- Lymphohistiocytic (10%): lymphoma cells are admixed with numerous reactive histiocytes that may obscure the lymphoma cells; lymphoma cells often cluster around vessels and are often smaller than in the common pattern
- Small cell (5-10%): predominant population of smaller lymphoma cells; hallmark cells are often concentrated around vessels; may also see "fried egg cells" (pale cytoplasm with central nucleus) or signet ring-like cells; can misdiagnose of peripheral T-cell lymphoma, NOS
- Hodgkin-like (3%): mimics nodular sclerosis classic Hodgkin lymphoma
- Composite (15%): more than one pattern in a single lymph node
When lymph node is only partially involved, lymphoma characteristically grows in the sinuses, which may mimic a metastatic tumor.
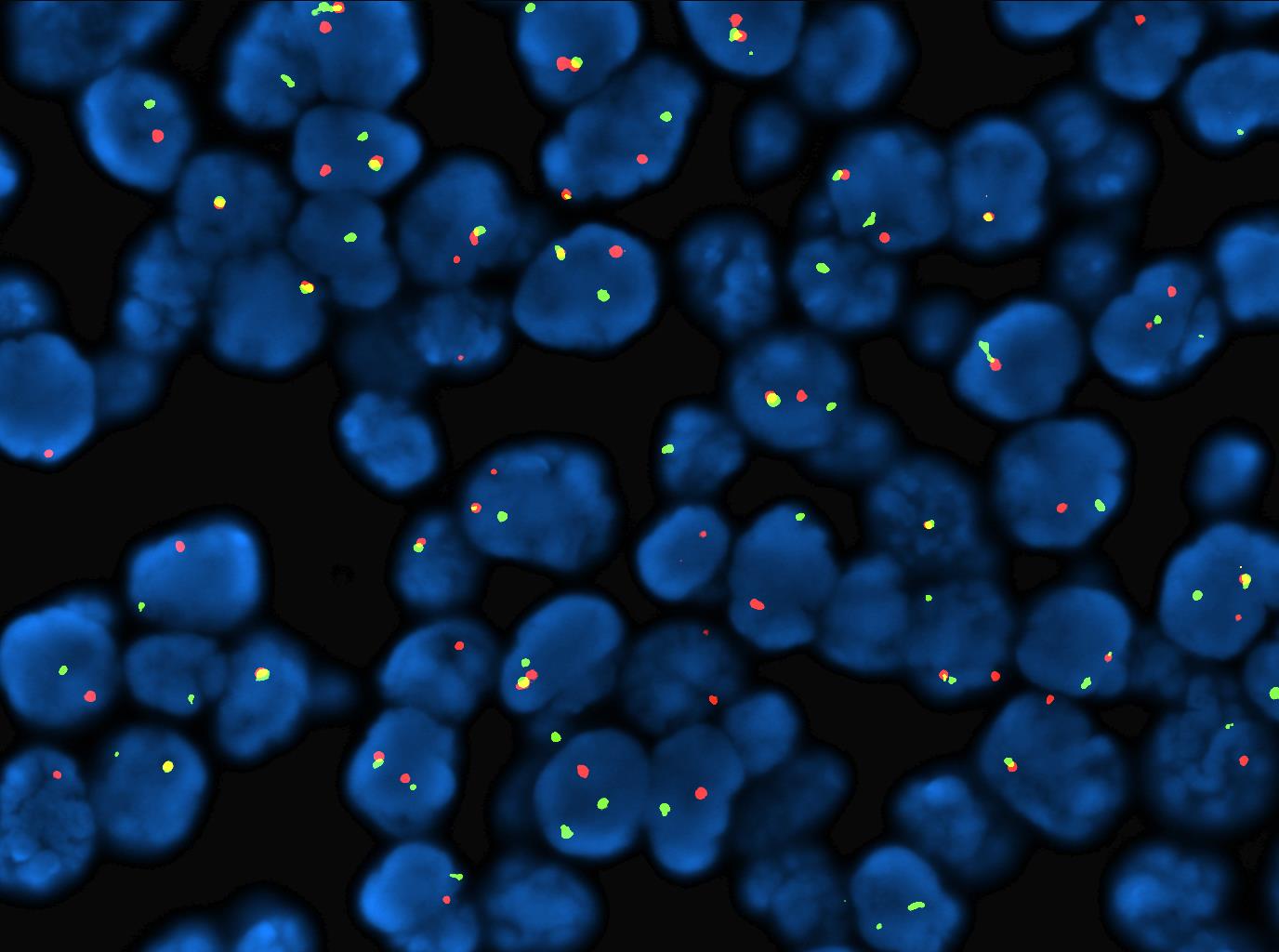
Immunophenotype
ALK+ ALCL show the following staining pattern[6][7]:
- CD30+: Cell membrane and Golgi; large lymphoma cells show strongest staining; smaller cells may show weak, partial to negative staining
- ALK+: cellular location of ALK staining varies depending on ALK translocation partner. In the most common t(2;5), most cases show both cytoplasmic and nuclear ALK staining. In the small cell variant, staining is usually restricted to the nucleus
- EMA+: some cases show positivity in only a proportion of lymphoma cells
- CD3(-): >75% of cases are CD3-negative
- CD4>>>CD8
- CD2 and CD5: Majority positive
- Cytotoxic marker(s)+: TIA1, granzyme B and/or perforin
- CD45: variably positive
- CD25+
- BCL2-negative
Chromosomal Rearrangements (Gene Fusions)
- ALK(+) ALCL is characterized by chromosomal translocations involving ALK gene, a receptor tyrosine kinase domain at 2p23.
- Approximately 80% of cases show a cytogenetic translocation t(2;5) (NPM1-ALK, t(2;5)(p23;q35)) which fuses the ALK gene to the nucleophosmine (NPM) gene at 5q35, resulting in the overexpression and constitutive activation of a chimeric ALK fusion protein, which plays an important role in ALK-mediated oncogenesis.[8]
- ALK translocations may be seen in multiple malignancies including epithelial malignancies[9][10][11][12][13][14], inflammatory myofibroblastic tumor[15][16][17], non-Hodgkin's lymphoma[18][19][20], and ALK+ histiocytosis [21][22][23].
Table below shows described ALK translocations with ALK staining pattern, and frequency of cases. Of note, identifying the ALK fusion partner is not considered necessary in routine clinical practice.
| Chromosomal
Anomaly |
ALK partner | ALK staining pattern | Percentage
of cases |
|---|---|---|---|
| t(2;5)(p23;q35) | NPM1 | Nuclear, nucleolar, diffuse cytoplasmic | 84% |
| t(1;2)(q25;p23)[24] | TPM3 | Diffuse cytoplasmic with peripheral intensification | 13% |
| inv(2)(p23q35)[25] | ATIC | Diffuse cytoplasmic | 1% |
| t(2;3)(p23;q12.2)[26] | TFG | Diffuse cytoplasmic | <1% |
| t(2;17)(p23;q23)[27] | CLTC | Granular cytoplasmic | <1% |
| t(X;2)(q11-22;p23)[28] | MSN | Membrane | <1% |
| t(2;19)(p23;p13.1)[29] | TPM4 | Diffuse cytoplasmic | <1% |
| t(2;22)(p23;q11.2)[30] | MYH9 | Diffuse cytoplasmic | <1% |
| t(2;17)(p23;q25)[29] | RNF213 | Diffuse cytoplasmic | <1% |
| t(2;9)(p23;q33)[31] | TRAF-1 | Diffuse cytoplasmic | <1% |
Characteristic Chromosomal Aberrations / Patterns
See other sections.
Genomic Gain/Loss/LOH
Frequent secondary chromosomal imbalances are seen in ALK+ ALCL (58% of cases), as based on comparative genomic hybridization analysis[32].
| Chromosome Number | Gain/Loss/Amp/LOH | Frequency | Comment |
|---|---|---|---|
| 2q | Gain | 12% | |
| 4q | Loss | 28% | |
| 11q22 (ATM) | Loss, LOH | 28% | |
| 13q | Loss | 28% | Also see in ALK- cases |
| 7p | Gain | 12% | Also seen in ALK- cases |
| 17p13 (TP53) | Gain | 28% | |
| 17p13 (TP53) | Loss[33] | 9% | More common in ALK- cases (42%) |
| 17q24-qter | Gain | 28% |
Gene Mutations (SNV/INDEL)
- Limited literature on somatic mutations in ALK+ ALCL
| Gene | Function or Presumed Mechanism | Frequency |
|---|---|---|
| LRP1B[34] | Tumor suppressor | 19% |
| NOTCH1[35] | Activating | 9.3% (p.Thr349Pro)
10.2% (p.Thr311Pro) |
| TP53[34] | Tumor suppressor | 11% |
- Epigenetic modifier genes: KMT2D, TET2, EP300, KMT2C[34]
- Other mutations: EPHA5
Negative genes mutations:
- JAK1, STAT3: Mutations described in ALK(-) ALCL[36], and breast implant-associated anaplastic large cell lymphoma (BIA-ALCL)[37]
- RHOA, DNMT3A, CD28: Mutations described in peripheral T cell-lymphoma (PTCL), NOS, and in angioimmunoblastic T-cell lymphoma (AITL)[38]
- IDH2 mutations are relatively specific for AITL[39][40]
A variety of mechanisms for the acquired resistance to ALK inhibitors, such as crizotinib, have been described:
- ALK kinase domain secondary mutations, including L1196 M, G1269A, L1152R, C1156Y, I1171T, F1174 L, G1202R, and S1206Y, have been identified as the key mechanism of resistance[41][42][43][44][45][46][47]
- The G1269A mutation, in which the glycine at 1269 is substituted with an alanine, causes steric hindrance, resulting in decreased affinity for crizotinib.[48][49]
- Gain in ALK copy number and loss of ALK gene rearrangement have also been implicated in the development of acquired resistance to crizotinib.[43][44][45]
Epigenomics (Methylation)
- NPM-ALK via STAT3-activated DNA methyltransferases[50] uses epigenetic silencing mechanisms to:
- Downregulate tumor suppressor genes to maintain its own expression (i.e. to inhibit downregulation of NPM-ALK). Silenced tumor suppressors include:
- Silence T-cell receptor complex and signaling pathway (CD3e, ZAP70, LAT, SLP76)[55]
- Histone H3 lysine 27 (H3K27) trimethylation silences promoters of important T-cell transcription factor genes (GATA3, TCF1 and LEF1)[56]
- Reader is directed to this review for more comprehensive review of epigenetics in peripheral T-cell lymphomas[57]
Genes and Main Pathways Involved
- Activation of the ALK catalytic domain leads to the oncogenic properties of the ALK protein, leading to activation of multiple signaling cascades including[58]:
- RAS-ERK
- JAK/STAT
- STAT3 is a pivotal transcription factor in most ALCL subtypes:
- NPM1/ALK and variants lead to expression of ALK fusion proteins with constitutive ALK tyrosine kinase activity, which converges in the activation of the downstream oncogenic transcription factor STAT3[36][38].
- In the absence of ALK fusions there are activation JAK1 and/or STAT3 mutations in ALK(-) ALCL [36], and some BIA-ALCL. [59].
- STAT3 is a pivotal transcription factor in most ALCL subtypes:
- PI3K/AKT/mTOR
- ALK-NPM-STAT3 induces:
- See Epigenomics section above
- TGF beta, IL-10, PD-L1/CD274 to create immunosuppressive microenvironment and evasion of immune system[60][61][62]
- ICOS expression (CD28 costimulatory receptor superfamily)
- HIF1α expression induces expression of VEGF (tumor angiogenesis); allows lymphoma cells to adapt to hypoxic conditions[63]
- Expression of embryonic genes (SOX2, SALL4) promoting stem cell-like program
- Deregulation of microRNAs (miR-155, miR-101, miR-17-92 cluster, miR-26a, miR-16)[64][65][66][67][68]
Diagnostic Testing Methods
- Diagnosis is based on histologic evaluation and immunohistochemical positivity for CD30 and ALK on the T-lymphoma cells.
- FISH using an ALK breakapart probe or karyotype analysis can detect ALK translocations, but is not required for diagnosis as it can be established by morphology and immunohistochemistry.
Clinical Significance (Diagnosis, Prognosis and Therapeutic Implications)
Diagnosis
- As stated above, the diagnosis is based on histology and immunohistochemistry
- FISH is not required for diagnosis in routine practice [69][70]
Prognosis
- ALK+ ALCL has a better survival rate compared to ALK-negative ALCL
- However, differences in patient age (younger in ALK+) may account for this better survival[71]
- Different ALK translocation partners do not have prognostic significance
- Survival is predicted by International Prognostic Index (IPI) with overall long term survival rate approaching 80%
- Detecting minimal residual disease by PCR for NPM1-ALK (not readily commercially available) in bone marrow and peripheral blood during treatment could identify patients at risk of relapse[72]
- Small-cell or lymphohistiocytic patterns tend to present with disseminated disease and have a less favorable prognosis than the common pattern[73]
- NOTCH1 may be a biomarker for risk of relapse[35]
Therapy
- CD30 expression on ALCL (ALK+ or ALK-) allows for targeted therapy[74]
- First-line therapy: Brentuximab (anti-CD30) vedotin + CHP (cyclophosphamide, doxorubicin, and prednisone)
- ALK inhibition (crizotinib) can be an effective 2nd-line therapeutic strategy as ALK is essential for the proliferation and survival of ALK+ ALCL cells[75][74][76]
- Drug resistance may develop due to:
- Mutations of the ALK gene impairing binding of the inhibitor[77]; other ALK inhibitors are not currently FDA-approved for use in ALK+ ALCL
- See also gene mutations section above
- Engagement of other cell signaling pathways
- Drug resistance may develop due to:
- Preclinical models suggest role of:
- Combination therapy with hypomethylating agents (such as azacitidine) and epigenetic modifying drugs (such as romidepsin, a histone deacetylase inhibitor)[78]
- Inhibitors of HSP90 and mTOR inhibition[77]
- NOTCH1 inhibition by γ-secretase inhibitors (GSI) in combination with crizotinib may provide synergistic anti-tumor activity, or as a single agent in ALK-inhibitor resistant cell lines[35]
Familial Forms
- None
Other Information
- None
Links
- See References.
References
- ↑ 1.0 1.1 1.2 Arber DA, et al., (2017). Anaplastic large cell lymphoma, ALK-positive, in World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues, Revised 4th edition. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Arber DA, Hasserjian RP, Le Beau MM, Orazi A, and Siebert R, Editors. IARC Press: Lyon, France, p413-418.
- ↑ Savage, Kerry J.; et al. (2008-06-15). "ALK- anaplastic large-cell lymphoma is clinically and immunophenotypically different from both ALK+ ALCL and peripheral T-cell lymphoma, not otherwise specified: report from the International Peripheral T-Cell Lymphoma Project". Blood. 111 (12): 5496–5504. doi:10.1182/blood-2008-01-134270. ISSN 1528-0020. PMID 18385450.
- ↑ M, Fraga; et al. (1995). "Bone marrow involvement in anaplastic large cell lymphoma. Immunohistochemical detection of minimal disease and its prognostic significance". PMID 7817951.
- ↑ Stein, H.; et al. (2000-12-01). "CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features". Blood. 96 (12): 3681–3695. ISSN 0006-4971. PMID 11090048.
- ↑ Benharroch, D.; et al. (1998-03-15). "ALK-positive lymphoma: a single disease with a broad spectrum of morphology". Blood. 91 (6): 2076–2084. ISSN 0006-4971. PMID 9490693.
- ↑ Montes-Mojarro, Ivonne A.; et al. (2018-04-04). "The Pathological Spectrum of Systemic Anaplastic Large Cell Lymphoma (ALCL)". Cancers. 10 (4): E107. doi:10.3390/cancers10040107. ISSN 2072-6694. PMC 5923362. PMID 29617304.
- ↑ Stein, H.; et al. (2000-12-01). "CD30(+) anaplastic large cell lymphoma: a review of its histopathologic, genetic, and clinical features". Blood. 96 (12): 3681–3695. ISSN 0006-4971. PMID 11090048.
- ↑ Morris, S. W.; et al. (1994-03-04). "Fusion of a kinase gene, ALK, to a nucleolar protein gene, NPM, in non-Hodgkin's lymphoma". Science (New York, N.Y.). 263 (5151): 1281–1284. doi:10.1126/science.8122112. ISSN 0036-8075. PMID 8122112.
- ↑ Holla, Vijaykumar R.; et al. (2017-1). "ALK: a tyrosine kinase target for cancer therapy". Cold Spring Harbor Molecular Case Studies. 3 (1): a001115. doi:10.1101/mcs.a001115. ISSN 2373-2873. PMC 5171696. PMID 28050598. Check date values in:
|date=(help) - ↑ Amatu, Alessio; et al. (2015-12-22). "Novel CAD-ALK gene rearrangement is drugable by entrectinib in colorectal cancer". British Journal of Cancer. 113 (12): 1730–1734. doi:10.1038/bjc.2015.401. ISSN 0007-0920. PMC 4701996. PMID 26633560.
- ↑ Camidge, D. Ross; et al. (2011-04). "Anaplastic lymphoma kinase gene rearrangements in non-small cell lung cancer are associated with prolonged progression-free survival on pemetrexed". Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer. 6 (4): 774–780. doi:10.1097/JTO.0b013e31820cf053. ISSN 1556-1380. PMC 3626562. PMID 21336183. Check date values in:
|date=(help) - ↑ Choi, Young Lim; et al. (2008-07-01). "Identification of novel isoforms of the EML4-ALK transforming gene in non-small cell lung cancer". Cancer Research. 68 (13): 4971–4976. doi:10.1158/0008-5472.CAN-07-6158. ISSN 1538-7445. PMID 18593892.
- ↑ Kelly, Lindsey M.; et al. (2014-03-18). "Identification of the transforming STRN-ALK fusion as a potential therapeutic target in the aggressive forms of thyroid cancer". Proceedings of the National Academy of Sciences of the United States of America. 111 (11): 4233–4238. doi:10.1073/pnas.1321937111. ISSN 0027-8424. PMC 3964116. PMID 24613930.
- ↑ Ambrosini, Margherita; et al. (2022-04). "ALK Inhibitors in Patients With ALK Fusion-Positive GI Cancers: An International Data Set and a Molecular Case Series". JCO precision oncology. 6: e2200015. doi:10.1200/PO.22.00015. ISSN 2473-4284. PMID 35476549 Check
|pmid=value (help). Check date values in:|date=(help) - ↑ Bridge, Julia A.; et al. (2001-8). "Fusion of the ALK Gene to the Clathrin Heavy Chain Gene, CLTC, in Inflammatory Myofibroblastic Tumor". The American Journal of Pathology. 159 (2): 411–415. ISSN 0002-9440. PMC 1850566. PMID 11485898. Check date values in:
|date=(help) - ↑ Lawrence, B.; et al. (2000-08). "TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic tumors". The American Journal of Pathology. 157 (2): 377–384. doi:10.1016/S0002-9440(10)64550-6. ISSN 0002-9440. PMC 1850130. PMID 10934142. Check date values in:
|date=(help) - ↑ Ma, Zhigui; et al. (2003-05). "Fusion of ALK to the Ran-binding protein 2 (RANBP2) gene in inflammatory myofibroblastic tumor". Genes, Chromosomes & Cancer. 37 (1): 98–105. doi:10.1002/gcc.10177. ISSN 1045-2257. PMID 12661011. Check date values in:
|date=(help) - ↑ Pan, Zenggang; et al. (2017-01). "ALK-positive Large B-cell Lymphoma: A Clinicopathologic Study of 26 Cases With Review of Additional 108 Cases in the Literature". The American Journal of Surgical Pathology. 41 (1): 25–38. doi:10.1097/PAS.0000000000000753. ISSN 1532-0979. PMID 27740969. Check date values in:
|date=(help) - ↑ Laurent, Camille; et al. (2009-09-01). "Anaplastic lymphoma kinase-positive diffuse large B-cell lymphoma: a rare clinicopathologic entity with poor prognosis". Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 27 (25): 4211–4216. doi:10.1200/JCO.2008.21.5020. ISSN 1527-7755. PMID 19636007.
- ↑ Sakamoto, Kana; et al. (2016-04). "ALK-positive large B-cell lymphoma: identification of EML4-ALK and a review of the literature focusing on the ALK immunohistochemical staining pattern". International Journal of Hematology. 103 (4): 399–408. doi:10.1007/s12185-016-1934-1. ISSN 1865-3774. PMID 26781614. Check date values in:
|date=(help) - ↑ Takeyasu, Yuki; et al. (2021). "Impact of ALK Inhibitors in Patients With ALK-Rearranged Nonlung Solid Tumors". JCO precision oncology. 5: PO.20.00383. doi:10.1200/PO.20.00383. ISSN 2473-4284. PMC 8140781 Check
|pmc=value (help). PMID 34036223 Check|pmid=value (help). - ↑ Chang, Kenneth Tou En; et al. (2019-05). "ALK-positive histiocytosis: an expanded clinicopathologic spectrum and frequent presence of KIF5B-ALK fusion". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 32 (5): 598–608. doi:10.1038/s41379-018-0168-6. ISSN 1530-0285. PMID 30573850. Check date values in:
|date=(help) - ↑ Chan, John K. C.; et al. (2008-10-01). "ALK+ histiocytosis: a novel type of systemic histiocytic proliferative disorder of early infancy". Blood. 112 (7): 2965–2968. doi:10.1182/blood-2008-03-147017. ISSN 1528-0020. PMID 18660380.
- ↑ Lamant, L.; et al. (1999-05-01). "A new fusion gene TPM3-ALK in anaplastic large cell lymphoma created by a (1;2)(q25;p23) translocation". Blood. 93 (9): 3088–3095. ISSN 0006-4971. PMID 10216106.
- ↑ Trinei, M.; et al. (2000-02-15). "A new variant anaplastic lymphoma kinase (ALK)-fusion protein (ATIC-ALK) in a case of ALK-positive anaplastic large cell lymphoma". Cancer Research. 60 (4): 793–798. ISSN 0008-5472. PMID 10706082.
- ↑ Hernández, L.; et al. (1999-11-01). "TRK-fused gene (TFG) is a new partner of ALK in anaplastic large cell lymphoma producing two structurally different TFG-ALK translocations". Blood. 94 (9): 3265–3268. ISSN 0006-4971. PMID 10556217.
- ↑ Touriol, C.; et al. (2000-05-15). "Further demonstration of the diversity of chromosomal changes involving 2p23 in ALK-positive lymphoma: 2 cases expressing ALK kinase fused to CLTCL (clathrin chain polypeptide-like)". Blood. 95 (10): 3204–3207. ISSN 0006-4971. PMID 10807789.
- ↑ Tort, F.; et al. (2001-03). "Molecular characterization of a new ALK translocation involving moesin (MSN-ALK) in anaplastic large cell lymphoma". Laboratory Investigation; a Journal of Technical Methods and Pathology. 81 (3): 419–426. doi:10.1038/labinvest.3780249. ISSN 0023-6837. PMID 11310834. Check date values in:
|date=(help) - ↑ 29.0 29.1 Cools, Jan; et al. (2002-08). "Identification of novel fusion partners of ALK, the anaplastic lymphoma kinase, in anaplastic large-cell lymphoma and inflammatory myofibroblastic tumor". Genes, Chromosomes & Cancer. 34 (4): 354–362. doi:10.1002/gcc.10033. ISSN 1045-2257. PMID 12112524. Check date values in:
|date=(help) - ↑ Lamant, Laurence; et al. (2003-08). "Non-muscle myosin heavy chain (MYH9): a new partner fused to ALK in anaplastic large cell lymphoma". Genes, Chromosomes & Cancer. 37 (4): 427–432. doi:10.1002/gcc.10232. ISSN 1045-2257. PMID 12800156. Check date values in:
|date=(help) - ↑ Feldman, Andrew L.; et al. (2013-11). "Novel TRAF1-ALK fusion identified by deep RNA sequencing of anaplastic large cell lymphoma". Genes, Chromosomes & Cancer. 52 (11): 1097–1102. doi:10.1002/gcc.22104. ISSN 1098-2264. PMID 23999969. Check date values in:
|date=(help) - ↑ I, Salaverria; et al. (2008). "Genomic profiling reveals different genetic aberrations in systemic ALK-positive and ALK-negative anaplastic large cell lymphomas". PMID 18275429.
- ↑ Boi, Michela; et al. (2013-10-10). "PRDM1/BLIMP1 is commonly inactivated in anaplastic large T-cell lymphoma". Blood. 122 (15): 2683–2693. doi:10.1182/blood-2013-04-497933. ISSN 0006-4971.
- ↑ 34.0 34.1 34.2 Lobello, Cosimo; et al. (2020-11-27). "STAT3 and TP53 mutations associate with poor prognosis in anaplastic large cell lymphoma". Leukemia: 1–6. doi:10.1038/s41375-020-01093-1. ISSN 1476-5551.
- ↑ 35.0 35.1 35.2 Larose, Hugo; et al. (04 23, 2020). "Whole Exome Sequencing reveals NOTCH1 mutations in anaplastic large cell lymphoma and points to Notch both as a key pathway and a potential therapeutic target". Haematologica. doi:10.3324/haematol.2019.238766. ISSN 1592-8721. PMID 32327503 Check
|pmid=value (help). Check date values in:|date=(help) - ↑ 36.0 36.1 36.2 Crescenzo, Ramona; et al. (2015-04-13). "Convergent mutations and kinase fusions lead to oncogenic STAT3 activation in anaplastic large cell lymphoma". Cancer Cell. 27 (4): 516–532. doi:10.1016/j.ccell.2015.03.006. ISSN 1878-3686. PMC 5898430. PMID 25873174.
- ↑ Blombery, Piers; et al. (2016-9). "Whole exome sequencing reveals activating JAK1 and STAT3 mutations in breast implant-associated anaplastic large cell lymphoma anaplastic large cell lymphoma". Haematologica. 101 (9): e387–e390. doi:10.3324/haematol.2016.146118. ISSN 0390-6078. PMC 5060038. PMID 27198716. Check date values in:
|date=(help) - ↑ 38.0 38.1 Sandell, Rosalind F.; et al. (2017-04). "Genetic Landscape and Classification of Peripheral T Cell Lymphomas". Current Oncology Reports. 19 (4): 28. doi:10.1007/s11912-017-0582-9. ISSN 1534-6269. PMC 5517131. PMID 28303495. Check date values in:
|date=(help) - ↑ Wang, Chao; et al. (2015-10-08). "IDH2R172 mutations define a unique subgroup of patients with angioimmunoblastic T-cell lymphoma". Blood. 126 (15): 1741–1752. doi:10.1182/blood-2015-05-644591. ISSN 1528-0020. PMC 4600014. PMID 26268241.
- ↑ Cairns, Rob A.; et al. (2012-02-23). "IDH2 mutations are frequent in angioimmunoblastic T-cell lymphoma". Blood. 119 (8): 1901–1903. doi:10.1182/blood-2011-11-391748. ISSN 1528-0020. PMC 3293643. PMID 22215888.
- ↑ Guérin, Annie; et al. (2015-06). "ALK rearrangement testing and treatment patterns for patients with ALK-positive non-small cell lung cancer". Cancer Epidemiology. 39 (3): 307–312. doi:10.1016/j.canep.2015.04.005. ISSN 1877-783X. PMID 25914136. Check date values in:
|date=(help) - ↑ Gainor, Justin F.; et al. (2013-08-01). "ALK rearrangements are mutually exclusive with mutations in EGFR or KRAS: an analysis of 1,683 patients with non-small cell lung cancer". Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 19 (15): 4273–4281. doi:10.1158/1078-0432.CCR-13-0318. ISSN 1557-3265. PMC 3874127. PMID 23729361.
- ↑ 43.0 43.1 Doebele, Robert C.; et al. (2012-03-01). "Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer". Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 18 (5): 1472–1482. doi:10.1158/1078-0432.CCR-11-2906. ISSN 1557-3265. PMC 3311875. PMID 22235099.
- ↑ 44.0 44.1 Isozaki, Hideko; et al. (2015-04-30). "Mechanisms of Acquired Resistance to ALK Inhibitors and the Rationale for Treating ALK-positive Lung Cancer". Cancers. 7 (2): 763–783. doi:10.3390/cancers7020763. ISSN 2072-6694. PMC 4491683. PMID 25941796.
- ↑ 45.0 45.1 Sasaki, Takaaki; et al. (2011-09-15). "A novel ALK secondary mutation and EGFR signaling cause resistance to ALK kinase inhibitors". Cancer Research. 71 (18): 6051–6060. doi:10.1158/0008-5472.CAN-11-1340. ISSN 1538-7445. PMC 3278914. PMID 21791641.
- ↑ Toyokawa, Gouji; et al. (2014-12). "Secondary mutations at I1171 in the ALK gene confer resistance to both Crizotinib and Alectinib". Journal of Thoracic Oncology: Official Publication of the International Association for the Study of Lung Cancer. 9 (12): e86–87. doi:10.1097/JTO.0000000000000358. ISSN 1556-1380. PMID 25393798. Check date values in:
|date=(help) - ↑ Li, Yanrong; et al. (2020-06). "Activation of IGF-1R pathway and NPM-ALK G1269A mutation confer resistance to crizotinib treatment in NPM-ALK positive lymphoma". Investigational New Drugs. 38 (3): 599–609. doi:10.1007/s10637-019-00802-7. ISSN 1573-0646. PMID 31177400. Check date values in:
|date=(help) - ↑ Friboulet, Luc; et al. (2014-06). "The ALK inhibitor ceritinib overcomes crizotinib resistance in non-small cell lung cancer". Cancer Discovery. 4 (6): 662–673. doi:10.1158/2159-8290.CD-13-0846. ISSN 2159-8290. PMC 4068971. PMID 24675041. Check date values in:
|date=(help) - ↑ Alshareef, Abdulraheem; et al. (2016-09-19). "The use of cellular thermal shift assay (CETSA) to study Crizotinib resistance in ALK-expressing human cancers". Scientific Reports. 6: 33710. doi:10.1038/srep33710. ISSN 2045-2322. PMC 5027386. PMID 27641368.
- ↑ Zhang, Qian; et al. (2006-08-01). "STAT3 induces transcription of the DNA methyltransferase 1 gene (DNMT1) in malignant T lymphocytes". Blood. 108 (3): 1058–1064. doi:10.1182/blood-2005-08-007377. ISSN 0006-4971. PMC 1895864. PMID 16861352.
- ↑ Zhang, Qian; et al. (2007-11). "STAT5A is epigenetically silenced by the tyrosine kinase NPM1-ALK and acts as a tumor suppressor by reciprocally inhibiting NPM1-ALK expression". Nature Medicine. 13 (11): 1341–1348. doi:10.1038/nm1659. ISSN 1078-8956. PMID 17922009. Check date values in:
|date=(help) - ↑ Zhang, Qian; et al. (2005-05-10). "STAT3- and DNA methyltransferase 1-mediated epigenetic silencing of SHP-1 tyrosine phosphatase tumor suppressor gene in malignant T lymphocytes". Proceedings of the National Academy of Sciences of the United States of America. 102 (19): 6948–6953. doi:10.1073/pnas.0501959102. ISSN 0027-8424. PMC 1100783. PMID 15870198.
- ↑ 53.0 53.1 Zhang, Qian; et al. (2011-07-19). "IL-2R common gamma-chain is epigenetically silenced by nucleophosphin-anaplastic lymphoma kinase (NPM-ALK) and acts as a tumor suppressor by targeting NPM-ALK". Proceedings of the National Academy of Sciences of the United States of America. 108 (29): 11977–11982. doi:10.1073/pnas.1100319108. ISSN 1091-6490. PMC 3141982. PMID 21715655.
- ↑ Hoareau-Aveilla, Coralie; et al. (2015-09). "Reversal of microRNA-150 silencing disadvantages crizotinib-resistant NPM-ALK(+) cell growth". The Journal of Clinical Investigation. 125 (9): 3505–3518. doi:10.1172/JCI78488. ISSN 1558-8238. PMC 4588301. PMID 26258416. Check date values in:
|date=(help) - ↑ Ambrogio, Chiara; et al. (2009-11-15). "NPM-ALK oncogenic tyrosine kinase controls T-cell identity by transcriptional regulation and epigenetic silencing in lymphoma cells". Cancer Research. 69 (22): 8611–8619. doi:10.1158/0008-5472.CAN-09-2655. ISSN 1538-7445. PMC 2784121. PMID 19887607.
- ↑ Joosten, Maria; et al. (2013-02). "Histone acetylation and DNA demethylation of T cells result in an anaplastic large cell lymphoma-like phenotype". Haematologica. 98 (2): 247–254. doi:10.3324/haematol.2011.054619. ISSN 1592-8721. PMC 3561432. PMID 22899583. Check date values in:
|date=(help) - ↑ Zhang, Ping; et al. (2020-11-07). "Epigenetic alterations and advancement of treatment in peripheral T-cell lymphoma". Clinical Epigenetics. 12 (1): 169. doi:10.1186/s13148-020-00962-x. ISSN 1868-7083. PMC 7648940 Check
|pmc=value (help). PMID 33160401 Check|pmid=value (help). - ↑ M, Boi; et al. (2015). "Advances in understanding the pathogenesis of systemic anaplastic large cell lymphomas". PMID 25559471.
- ↑ Di Napoli, Arianna; et al. (2018-03). "Targeted next generation sequencing of breast implant-associated anaplastic large cell lymphoma reveals mutations in JAK/STAT signalling pathway genes, TP53 and DNMT3A". British Journal of Haematology. 180 (5): 741–744. doi:10.1111/bjh.14431. ISSN 1365-2141. PMID 27859003. Check date values in:
|date=(help) - ↑ Marzec, Michal; et al. (2008-12-30). "Oncogenic kinase NPM/ALK induces through STAT3 expression of immunosuppressive protein CD274 (PD-L1, B7-H1)". Proceedings of the National Academy of Sciences of the United States of America. 105 (52): 20852–20857. doi:10.1073/pnas.0810958105. ISSN 1091-6490. PMC 2634900. PMID 19088198.
- ↑ Kasprzycka, Monika; et al. (2008-08-15). "Gamma c-signaling cytokines induce a regulatory T cell phenotype in malignant CD4+ T lymphocytes". Journal of Immunology (Baltimore, Md.: 1950). 181 (4): 2506–2512. doi:10.4049/jimmunol.181.4.2506. ISSN 1550-6606. PMC 2586884. PMID 18684941.
- ↑ Yamamoto, Ryo; et al. (2009-11). "B7-H1 expression is regulated by MEK/ERK signaling pathway in anaplastic large cell lymphoma and Hodgkin lymphoma". Cancer Science. 100 (11): 2093–2100. doi:10.1111/j.1349-7006.2009.01302.x. ISSN 1349-7006. PMID 19703193. Check date values in:
|date=(help) - ↑ Martinengo, Cinzia; et al. (2014-11-01). "ALK-dependent control of hypoxia-inducible factors mediates tumor growth and metastasis". Cancer Research. 74 (21): 6094–6106. doi:10.1158/0008-5472.CAN-14-0268. ISSN 1538-7445. PMID 25193384.
- ↑ Rodriguez, Antony; et al. (2007-04-27). "Requirement of bic/microRNA-155 for normal immune function". Science (New York, N.Y.). 316 (5824): 608–611. doi:10.1126/science.1139253. ISSN 1095-9203. PMC 2610435. PMID 17463290.
- ↑ Merkel, Olaf; et al. (2010-09-14). "Identification of differential and functionally active miRNAs in both anaplastic lymphoma kinase (ALK)+ and ALK- anaplastic large-cell lymphoma". Proceedings of the National Academy of Sciences of the United States of America. 107 (37): 16228–16233. doi:10.1073/pnas.1009719107. ISSN 1091-6490. PMC 2941277. PMID 20805506.
- ↑ Spaccarotella, Elisa; et al. (2014-01). "STAT3-mediated activation of microRNA cluster 17~92 promotes proliferation and survival of ALK-positive anaplastic large cell lymphoma". Haematologica. 99 (1): 116–124. doi:10.3324/haematol.2013.088286. ISSN 1592-8721. PMC 4007939. PMID 23975180. Check date values in:
|date=(help) - ↑ Zhu, Haifeng; et al. (2013-05). "NPM-ALK up-regulates iNOS expression through a STAT3/microRNA-26a-dependent mechanism". The Journal of Pathology. 230 (1): 82–94. doi:10.1002/path.4171. ISSN 1096-9896. PMC 3940725. PMID 23338972. Check date values in:
|date=(help) - ↑ Dejean, E.; et al. (2011-12). "Hypoxia-microRNA-16 downregulation induces VEGF expression in anaplastic lymphoma kinase (ALK)-positive anaplastic large-cell lymphomas". Leukemia. 25 (12): 1882–1890. doi:10.1038/leu.2011.168. ISSN 1476-5551. PMID 21778999. Check date values in:
|date=(help) - ↑ Falini, B.; et al. (1998-09). "ALK expression defines a distinct group of T/null lymphomas ("ALK lymphomas") with a wide morphological spectrum". The American Journal of Pathology. 153 (3): 875–886. doi:10.1016/S0002-9440(10)65629-5. ISSN 0002-9440. PMC 1853018. PMID 9736036. Check date values in:
|date=(help) - ↑ Pittaluga, S.; et al. (1997-08). "The monoclonal antibody ALK1 identifies a distinct morphological subtype of anaplastic large cell lymphoma associated with 2p23/ALK rearrangements". The American Journal of Pathology. 151 (2): 343–351. ISSN 0002-9440. PMC 1858018. PMID 9250148. Check date values in:
|date=(help) - ↑ D, Sibon; et al. (2012). "Long-term outcome of adults with systemic anaplastic large-cell lymphoma treated within the Groupe d'Etude des Lymphomes de l'Adulte trials". PMID 23045585.
- ↑ C, Damm-Welk; et al. (2014). "Early assessment of minimal residual disease identifies patients at very high relapse risk in NPM-ALK-positive anaplastic large-cell lymphoma". PMID 24297868.
- ↑ L, Lamant; et al. (2011). "Prognostic impact of morphologic and phenotypic features of childhood ALK-positive anaplastic large-cell lymphoma: results of the ALCL99 study". PMID 22084369.
- ↑ 74.0 74.1 National Comprehensive Cancer Network (January 2021). "NCCN Clinical Practice Guidelines in Oncology: T-cell lymphomas" (PDF).CS1 maint: display-authors (link)
- ↑ Werner, Michael T.; et al. (02 16, 2017). "Nucleophosmin-anaplastic lymphoma kinase: the ultimate oncogene and therapeutic target". Blood. 129 (7): 823–831. doi:10.1182/blood-2016-05-717793. ISSN 1528-0020. PMID 27879258. Check date values in:
|date=(help) - ↑ Food and Drug Administration (January 2021). "FDA approves crizotinib for children and young adults with relapsed or refractory, systemic anaplastic large cell lymphoma".CS1 maint: display-authors (link)
- ↑ 77.0 77.1 Zdzalik, Daria; et al. (2014-04). "Activating mutations in ALK kinase domain confer resistance to structurally unrelated ALK inhibitors in NPM-ALK-positive anaplastic large-cell lymphoma". Journal of Cancer Research and Clinical Oncology. 140 (4): 589–598. doi:10.1007/s00432-014-1589-3. ISSN 1432-1335. PMC 3949014. PMID 24509625. Check date values in:
|date=(help) - ↑ Rozati, Sima; et al. (2016-04-15). "Romidepsin and Azacitidine Synergize in their Epigenetic Modulatory Effects to Induce Apoptosis in CTCL". Clinical Cancer Research: An Official Journal of the American Association for Cancer Research. 22 (8): 2020–2031. doi:10.1158/1078-0432.CCR-15-1435. ISSN 1557-3265. PMID 26660520.
Notes
*Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the CCGA coordinators (contact information provided on the homepage). Additional global feedback or concerns are also welcome.