BRST5:Tall cell carcinoma with reversed polarity
Primary Author(s)*
H. Evin Gulbahce, MD, MSCI, University of Utah, UT, and Katherine Geiersbach, MD, Mayo Clinic
Cancer Category/Type
Breast cancer / Epithelial Tumours of the Breast
Cancer Sub-Classification / Subtype
Tall cell carcinoma with reversed polarity
Definition / Description of Disease
Tall cell carcinoma with reversed polarity is a rare variant of invasive breast carcinoma with unusual histopathologic features. In 2019, 5th edition of the World Health Organization (WHO) classification of breast tumors, it is in the group of rare and salivary gland-type tumors and is associated with favorable prognosis.
Synonyms / Terminology
- Breast tumor resembling tall cell variant of papillary thyroid carcinoma
- Solid papillary breast carcinoma resembling the tall cell variant of papillary thyroid neoplasms (Historical)
- Breast cancer with altered nuclear polarity (Historical)
- Solid papillary carcinoma with reverse polarity (Historical)
- Tall cell variant of papillary breast carcinoma (Historical)
Epidemiology / Prevalence
Rare; fewer than 100 cases reported. No specific epidemiologic data are available. All patients have been women with a mean age of 64 years.
Clinical Features
| Signs and Symptoms | Mammographic or palpable mass
Axillary lymph node metastasis (rare; reported in only three patients) |
| Laboratory Findings | Not applicable |
Sites of Involvement
There is no specific predilection for location in the breast.
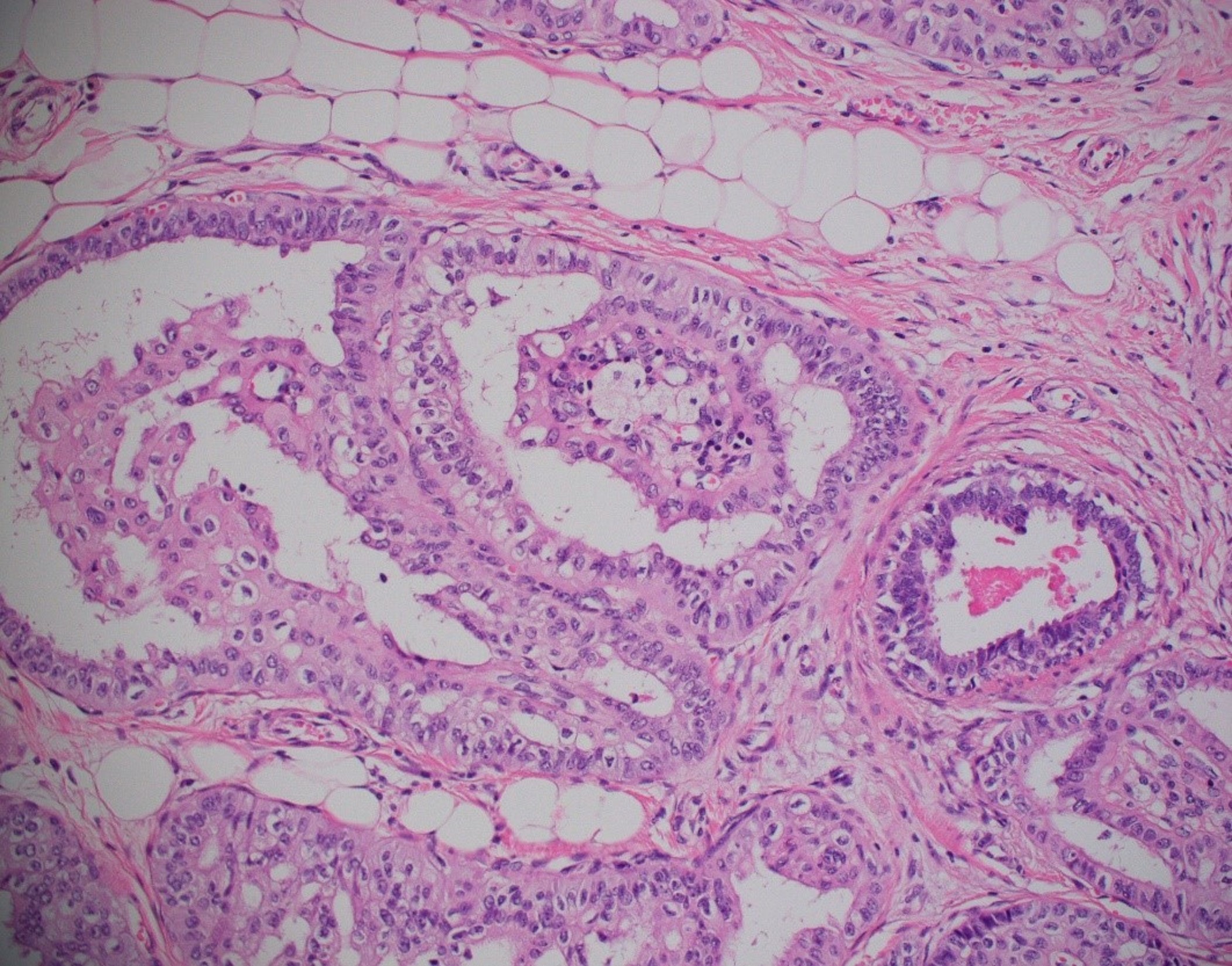
Morphologic Features
- Circumscribed nests of cells, many of which have fibrovascular cores. Foamy histiocytes are often present within the fibrovascular cores.
- Occasionally true papillae and cyst-like structures with colloid-like material are identified.
- Epithelial cells are tall, may have nuclear grooves and intranuclear cytoplasmic inclusions.
- The most characteristic feature is the presence of nuclei in the apical rather than basal pole of the cells hence the “reverse polarity”.
Immunophenotype
- Most carcinomas do not express estrogen or progesterone receptors (ER, PR). Those that tend to show staining of only a small fraction of the cells.
- No cases reported to be HER2 positive (3+) or amplified by ISH.
- Proliferative index (Ki67) has been less than 20%.
| Finding | Marker |
|---|---|
| Positive (universal) | Cytokeratin 7, cytokeratin 5/6 |
| Positive (subset) | GCDFP-15, GATA3, IDH1/2 mutant[1], calretinin |
| Negative (universal) | HER2 (ERBB2) expression or amplification; TTF-1, thyroglobulin, myoepithelial markers (p63, myosin) |
| Negative (subset) |
Chromosomal Rearrangements (Gene Fusions)
| Chromosomal Rearrangement | Genes in Fusion (5’ or 3’ Segments) | Pathogenic Derivative | Prevalence | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|
| N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
Individual Region Genomic Gain/Loss/LOH
| Chr # | Gain / Loss / Amp / LOH | Minimal Region Genomic Coordinates [Genome Build] | Minimal Region Cytoband | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|
| N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
Characteristic Chromosomal Patterns
| Chromosomal Pattern | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|
| N/A | N/A | N/A | N/A | N/A |
Gene Mutations (SNV/INDEL)
| Gene; Genetic Alteration | Presumed Mechanism (Tumor Suppressor Gene [TSG] / Oncogene / Other) | Prevalence (COSMIC / TCGA / Other) | Concomitant Mutations | Mutually Exclusive Mutations | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|---|
| IDH2 codon 172 mutations[2][3][4] | Gain of function (Oncogene) | <1 % (TCGA) | PIK3CA (most commonly H1047R), PIK3R1 | * | Yes | No | No | 90% of cases show IDH2 hot spot mutation.
No targeted therapy for IDH2 mutated breast cancer.
|
*A single case without IDH2 mutation but with a TET2 Q548* truncating mutation and with a PIK3CA H1047R mutation has been reported in one study.[2]
Note: A more extensive list of mutations can be found in cBioportal (https://www.cbioportal.org/), COSMIC (https://cancer.sanger.ac.uk/cosmic), ICGC (https://dcc.icgc.org/) and/or other databases. When applicable, gene-specific pages within the CCGA site directly link to pertinent external content.
Epigenomic Alterations
Global DNA hypermethylation
Genes and Main Pathways Involved
Put your text here and fill in the table
| Gene; Genetic Alteration | Pathway | Pathophysiologic Outcome |
|---|---|---|
| IDH2 codon 172 mutations (majority are R172S, R172T; other mutations include R172G, R172W, R172I)[5][3][2][4] | Carbon metabolism: citrate cycle | Increased conversion of α-ketoglutarate (α-KG) to the oncometabolite R-2-hydroxylglutarate (R-2-HG). Increased levels of 2-HG result in hypermethylation of epigenetic targets and a subsequent block in cellular differentiation. Due to widespread hypermethylation, there is increased H3K27me3 nuclear immunoreactivity in tumors harboring IDH2 R172 mutations. |
| PIK3CA mutations: H1047R most common[3] | PI3K/AKT/mTOR pathway | Three most common PIK3CA mutations are H1047R, E542K, and E545K; PIK3CA mutations induce hyperactivation of the alpha isoform of the catalytic subunit (p110α) of class IA PI3K kinase. Mutations are often co-occurring with other drivers in ER-positive breast cancers and are associated with endocrine resistance. PIK3CA mutations are targetable with the PI3K inhibitor alpelisib in ER positive breast cancers; however, tall cell carcinoma with reverse polarity is usually ER negative. |
Genetic Diagnostic Testing Methods
Next generation sequencing (NGS); immunohistochemistry with monoclonal antibodies against IDH2 mutant codon R172S (monoclonal antibody clone 11C8B1 is reactive against R172S or R172T); pyrosequencing; Sanger sequencing; PCR with allele detection (examples include PCR with melting curve analysis, or PCR with use of allele-specific probes); allele-specific PCR; single base extension.
Familial Forms
None
Additional Information
Links
References
- ↑ Pareja, Fresia; et al. (2020-06). "Immunohistochemical analysis of IDH2 R172 hotspot mutations in breast papillary neoplasms: applications in the diagnosis of tall cell carcinoma with reverse polarity". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 33 (6): 1056–1064. doi:10.1038/s41379-019-0442-2. ISSN 1530-0285. PMC 7286791 Check
|pmc=value (help). PMID 31896809. Check date values in:|date=(help) - ↑ Jump up to: 2.0 2.1 2.2 Chiang, Sarah; et al. (2016-12-15). "IDH2 Mutations Define a Unique Subtype of Breast Cancer with Altered Nuclear Polarity". Cancer Research. 76 (24): 7118–7129. doi:10.1158/0008-5472.CAN-16-0298. ISSN 1538-7445. PMC 5502804. PMID 27913435.
- ↑ Jump up to: 3.0 3.1 3.2 Lozada, John R.; et al. (2018-08). "Solid papillary breast carcinomas resembling the tall cell variant of papillary thyroid neoplasms (solid papillary carcinomas with reverse polarity) harbour recurrent mutations affecting IDH2 and PIK3CA: a validation cohort". Histopathology. 73 (2): 339–344. doi:10.1111/his.13522. ISSN 1365-2559. PMC 6783257. PMID 29603332. Check date values in:
|date=(help) - ↑ Jump up to: 4.0 4.1 Alsadoun, Nadjla; et al. (2018-09). "Solid papillary carcinoma with reverse polarity of the breast harbors specific morphologic, immunohistochemical and molecular profile in comparison with other benign or malignant papillary lesions of the breast: a comparative study of 9 additional cases". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 31 (9): 1367–1380. doi:10.1038/s41379-018-0047-1. ISSN 1530-0285. PMID 29785016. Check date values in:
|date=(help) - ↑ Zhong, Elaine; et al. (2019-04). "Breast Tumor Resembling the Tall Cell Variant of Papillary Thyroid Carcinoma: Molecular Characterization by Next-Generation Sequencing and Histopathological Comparison With Tall Cell Papillary Carcinoma of Thyroid". International Journal of Surgical Pathology. 27 (2): 134–141. doi:10.1177/1066896918800779. ISSN 1940-2465. PMID 30227763. Check date values in:
|date=(help)
Notes
*Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the CCGA coordinators (contact information provided on the homepage). Additional global feedback or concerns are also welcome.