Difference between revisions of "BRST5:Adenoid cystic carcinoma"
| [checked revision] | [checked revision] |
Kgeiersbach (talk | contribs) |
m (Jennelleh moved page BRST5:Adenoid Cystic Carcinoma to BRST5:Adenoid cystic carcinoma without leaving a redirect) |
||
| (10 intermediate revisions by 2 users not shown) | |||
| Line 41: | Line 41: | ||
==Morphologic Features== | ==Morphologic Features== | ||
| − | + | Tubular, cribriform, and solid patterns are observed. | |
| + | The classic subtype contains epithelial and myoepithelial cells with spaces called pseudolamina that contain stromal matrix with stromal cells (endothelial cells, fibroblasts) and basement membrane material (stains positive for collagen IV and laminin). Two cell populations are observed: an epithelial component that stains with low molecular weight cytokeratins (CK7, CK8), EMA, and sometimes CK5/6, and a myoepithelial component that stains with high molecular weight cytokeratins (CK14, CK5/6, p63) and typically also with myoepithelial markers (heavy-chain myosin, calponin, S100, CD10). | ||
| + | |||
| + | The solid basaloid subtype contains solid nests of basaloid cells with high grade nuclear features (marked nuclear atypia, high mitotic count, and necrosis). | ||
| + | |||
| + | Rare cases of adenoid cystic carcinoma can undergo high-grade transformation. | ||
==Immunophenotype== | ==Immunophenotype== | ||
| Line 61: | Line 66: | ||
==Chromosomal Rearrangements (Gene Fusions)== | ==Chromosomal Rearrangements (Gene Fusions)== | ||
| − | Recurrent rearrangements of ''MYB'' (or, more rarely, the paralogous gene ''MYBL1'') preserve the N-terminal DNA binding domain and transactivation domain in the chimeric gene product. The C-terminal regulatory domains of ''MYB'' or ''MYBL1'' is generally absent in the active fusion, but the intact gene sequence is preserved in reported cases of ''MYB'' amplification and in some ''MYBL1'' rearrangements.<ref name=":1">{{Cite journal|last=Persson|first=Marta|last2=Andrén|first2=Ywonne|last3=Mark|first3=Joachim|last4=Horlings|first4=Hugo M.|last5=Persson|first5=Fredrik|last6=Stenman|first6=Göran|date=2009-11-03|title=Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck|url=https://pubmed.ncbi.nlm.nih.gov/19841262|journal=Proceedings of the National Academy of Sciences of the United States of America|volume=106|issue=44|pages=18740–18744|doi=10.1073/pnas.0909114106|issn=1091-6490|pmc=2773970|pmid=19841262}}</ref><ref name=":2">{{Cite journal|last=Kim|first=Jisun|last2=Geyer|first2=Felipe C.|last3=Martelotto|first3=Luciano G.|last4=Ng|first4=Charlotte Ky|last5=Lim|first5=Raymond S.|last6=Selenica|first6=Pier|last7=Li|first7=Anqi|last8=Pareja|first8=Fresia|last9=Fusco|first9=Nicola|date=2018-02|title=MYBL1 rearrangements and MYB amplification in breast adenoid cystic carcinomas lacking the MYB-NFIB fusion gene|url=https://pubmed.ncbi.nlm.nih.gov/29149504|journal=The Journal of Pathology|volume=244|issue=2|pages=143–150|doi=10.1002/path.5006|issn=1096-9896|pmc=5839480|pmid=29149504}}</ref> Single cases of other fusions have been reported, including a ''KMT2C''::''WEE2'' fusion reported by Schwartz and others<ref>{{Cite journal|last=Schwartz|first=Christopher J.|last2=Brogi|first2=Edi|last3=Marra|first3=Antonio|last4=Da Cruz Paula|first4=Arnaud F.|last5=Nanjangud|first5=Gouri J.|last6=da Silva|first6=Edaise M.|last7=Patil|first7=Sujata|last8=Shah|first8=Shreena|last9=Ventura|first9=Katia|date=2022-02|title=The clinical behavior and genomic features of the so-called adenoid cystic carcinomas of the solid variant with basaloid features|url=https://pubmed.ncbi.nlm.nih.gov/34599282|journal=Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc|volume=35|issue=2|pages=193–201|doi=10.1038/s41379-021-00931-6|issn=1530-0285|pmc=9197148|pmid=34599282}}</ref>, | + | Recurrent rearrangements of ''MYB'' (or, more rarely, the paralogous gene ''MYBL1'') preserve the N-terminal DNA binding domain and transactivation domain in the chimeric gene product. The C-terminal regulatory domains of ''MYB'' or ''MYBL1'' is generally absent in the active fusion, but the intact gene sequence is preserved in reported cases of ''MYB'' amplification and in some ''MYBL1'' rearrangements.<ref name=":1">{{Cite journal|last=Persson|first=Marta|last2=Andrén|first2=Ywonne|last3=Mark|first3=Joachim|last4=Horlings|first4=Hugo M.|last5=Persson|first5=Fredrik|last6=Stenman|first6=Göran|date=2009-11-03|title=Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck|url=https://pubmed.ncbi.nlm.nih.gov/19841262|journal=Proceedings of the National Academy of Sciences of the United States of America|volume=106|issue=44|pages=18740–18744|doi=10.1073/pnas.0909114106|issn=1091-6490|pmc=2773970|pmid=19841262}}</ref><ref name=":2">{{Cite journal|last=Kim|first=Jisun|last2=Geyer|first2=Felipe C.|last3=Martelotto|first3=Luciano G.|last4=Ng|first4=Charlotte Ky|last5=Lim|first5=Raymond S.|last6=Selenica|first6=Pier|last7=Li|first7=Anqi|last8=Pareja|first8=Fresia|last9=Fusco|first9=Nicola|date=2018-02|title=MYBL1 rearrangements and MYB amplification in breast adenoid cystic carcinomas lacking the MYB-NFIB fusion gene|url=https://pubmed.ncbi.nlm.nih.gov/29149504|journal=The Journal of Pathology|volume=244|issue=2|pages=143–150|doi=10.1002/path.5006|issn=1096-9896|pmc=5839480|pmid=29149504}}</ref> Single cases of other fusions have been reported, including a ''KMT2C''::''WEE2'' fusion reported by Schwartz and others<ref name=":8">{{Cite journal|last=Schwartz|first=Christopher J.|last2=Brogi|first2=Edi|last3=Marra|first3=Antonio|last4=Da Cruz Paula|first4=Arnaud F.|last5=Nanjangud|first5=Gouri J.|last6=da Silva|first6=Edaise M.|last7=Patil|first7=Sujata|last8=Shah|first8=Shreena|last9=Ventura|first9=Katia|date=2022-02|title=The clinical behavior and genomic features of the so-called adenoid cystic carcinomas of the solid variant with basaloid features|url=https://pubmed.ncbi.nlm.nih.gov/34599282|journal=Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc|volume=35|issue=2|pages=193–201|doi=10.1038/s41379-021-00931-6|issn=1530-0285|pmc=9197148|pmid=34599282}}</ref>, |
{| class="wikitable sortable" | {| class="wikitable sortable" | ||
|- | |- | ||
| Line 101: | Line 106: | ||
| | | | ||
| | | | ||
| − | |Fusions involving ''MYBL1'' with other gene partners or more complex structural abnormalities associated with ''MYBL1'' gene fusion generate more complex karyotypes. Other reported ''MYBL1'' gene partners include ''ACTN1''<ref name=":2" />. | + | |Fusions involving ''MYBL1'' with other gene partners or more complex structural abnormalities associated with ''MYBL1'' gene fusion generate more complex karyotypes. Other reported ''MYBL1'' gene partners include ''ACTN1''<ref name=":2" />. |
|} | |} | ||
| Line 162: | Line 167: | ||
!Notes | !Notes | ||
|- | |- | ||
| − | |''NOTCH1'', ''NOTCH2'', and ''NOTCH3''; | + | |''NOTCH1'', ''NOTCH2'', and ''NOTCH3''; sequence variants <ref name=":5">{{Cite journal|last=Massé|first=Julie|last2=Truntzer|first2=Caroline|last3=Boidot|first3=Romain|last4=Khalifa|first4=Emmanuel|last5=Pérot|first5=Gaëlle|last6=Velasco|first6=Valérie|last7=Mayeur|first7=Laétitia|last8=Billerey-Larmonier|first8=Claire|last9=Blanchard|first9=Larry|date=2020-06|title=Solid-type adenoid cystic carcinoma of the breast, a distinct molecular entity enriched in NOTCH and CREBBP mutations|url=https://pubmed.ncbi.nlm.nih.gov/31857685|journal=Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc|volume=33|issue=6|pages=1041–1055|doi=10.1038/s41379-019-0425-3|issn=1530-0285|pmid=31857685}}</ref> |
|Gain of function | |Gain of function | ||
| + | |22-28% solid basaloid subtype <ref name=":8" /> <ref name=":5" /> | ||
| + | | | ||
| + | | | ||
| + | | | ||
| + | | | ||
| | | | ||
| + | |Mostly solid basaloid subtype, with poorer prognosis <ref name=":8" /> NOTCH mutations cause resistance to BET bromodomain inhibitors<br /> | ||
| + | |- | ||
| + | |''CREBBP''; inactivating sequence variants <ref name=":5" /> | ||
| + | |Loss of function | ||
| + | |17-33% solid basaloid subtype <ref name=":8" /><ref name=":5" /> | ||
| | | | ||
| | | | ||
| Line 170: | Line 185: | ||
| | | | ||
| | | | ||
| − | |Mostly solid basaloid subtype | + | |Mostly solid basaloid subtype, with poorer prognosis |
|- | |- | ||
| − | |'' | + | |''KMT2C''; inactivating sequence variants, deletion <ref name=":5" /> |
|Loss of function | |Loss of function | ||
| + | |22% solid basaloid subtype in one study <ref name=":8" /> | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
| + | | | ||
| + | |Mostly solid basaloid subtype, with poorer prognosis | ||
| + | |- | ||
| + | |''KDM6A''; inactivating sequence variants | ||
| + | |Loss of function | ||
| + | |22% solid basaloid subtype in one study <ref name=":8" /> | ||
| | | | ||
| | | | ||
| − | |Mostly solid basaloid subtype | + | | |
| + | | | ||
| + | | | ||
| + | |Mostly solid basaloid subtype, with poorer prognosis | ||
|- | |- | ||
|''CDK12''; missense<ref name=":5" /> | |''CDK12''; missense<ref name=":5" /> | ||
|Loss of function | |Loss of function | ||
| + | |38% solid basaloid subtype in one study <ref name=":5" /> | ||
| | | | ||
| | | | ||
| Line 189: | Line 215: | ||
| | | | ||
| | | | ||
| − | | | + | |Mostly solid basaloid subtype, with poorer prognosis |
| − | |||
|} | |} | ||
Note: A more extensive list of mutations can be found in cBioportal (https://www.cbioportal.org/), COSMIC (https://cancer.sanger.ac.uk/cosmic), ICGC (https://dcc.icgc.org/) and/or other databases. | Note: A more extensive list of mutations can be found in cBioportal (https://www.cbioportal.org/), COSMIC (https://cancer.sanger.ac.uk/cosmic), ICGC (https://dcc.icgc.org/) and/or other databases. | ||
| Line 213: | Line 238: | ||
|''NOTCH1'', ''NOTCH2'', ''NOTCH3'' | |''NOTCH1'', ''NOTCH2'', ''NOTCH3'' | ||
|NOTCH signaling | |NOTCH signaling | ||
| − | | | + | |Promotes cellular proliferation |
| − | |||
| − | |||
| − | |||
| − | |||
|} | |} | ||
| + | A study of adenoid cystic carcinoma of salivary glands by Drier and others delineates the mechanism of ''MYB'' gene pathway upregulation via rearrangements that increase MYB expression. ''MYB'' rearrangements typically juxtapose ''MYB'' with strong enhancers in regions downstream of ''NFIB, TGFBR3'' and ''RAD51B.'' Gene fusions most often occur on the 3' side of ''MYB'', a subset of gene fusions occur on the 5' side, and all serve to bring the ''MYB'' gene locus close to strong enhancer elements, thus upregulating MYB expression. The authors note that TP63 signaling is active in the myoepithelial component of low grade adenoid cystic carcinomas, while Notch signaling is active in luminal epithelial components. Furthermore, the authors suggest that Notch pathway mutations may underlie the switch to solid histology and the more aggressive clinical course of these tumors.<ref>{{Cite journal|last=Drier|first=Yotam|last2=Cotton|first2=Matthew J.|last3=Williamson|first3=Kaylyn E.|last4=Gillespie|first4=Shawn M.|last5=Ryan|first5=Russell J. H.|last6=Kluk|first6=Michael J.|last7=Carey|first7=Christopher D.|last8=Rodig|first8=Scott J.|last9=Sholl|first9=Lynette M.|date=2016-03|title=An oncogenic MYB feedback loop drives alternate cell fates in adenoid cystic carcinoma|url=https://pubmed.ncbi.nlm.nih.gov/26829750|journal=Nature Genetics|volume=48|issue=3|pages=265–272|doi=10.1038/ng.3502|issn=1546-1718|pmc=4767593|pmid=26829750}}</ref> | ||
| + | |||
==Genetic Diagnostic Testing Methods== | ==Genetic Diagnostic Testing Methods== | ||
FISH for MYB rearrangement; RT-PCR for MYB-NFIB fusion transcript; RNA-based sequencing (whole transcriptome or targeted) | FISH for MYB rearrangement; RT-PCR for MYB-NFIB fusion transcript; RNA-based sequencing (whole transcriptome or targeted) | ||
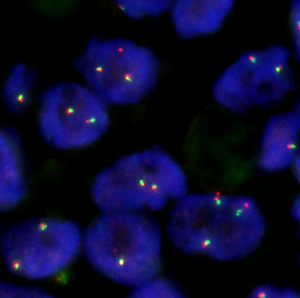
| + | [[File:MYB FISH break-apart probe.png|none|thumb|FISH with a break-apart probe targeting the 5' (red) and 3' (green) ''MYB'' gene region. Juxtaposed red and green signals indicate alleles with an intact ''MYB'' gene locus, and split / separated red and green signals indicate alleles with ''MYB'' rearrangement. The separation in this case is small, suggesting an inversion (i.e., intrachromosomal rearrangement).]] | ||
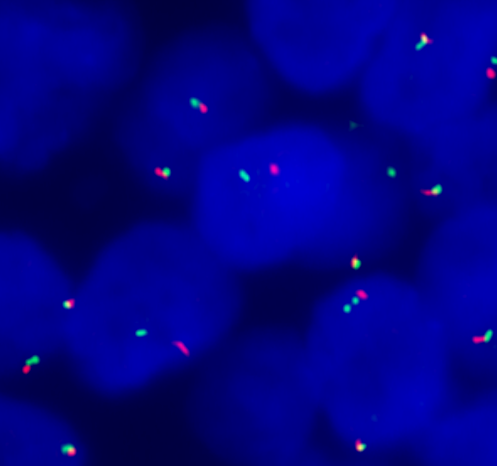
| + | [[File:Negative MYB FISH.tif|none|thumb|FISH with a break-apart probe targeting the 5' (red) and 3' (green) ''MYB'' gene region. This sample was negative for ''MYB'' rearrangement, and the majority of cells showed 1-3 fused red/green signals (juxtaposed red and green probe signals), consistent with an intact (unrearranged) ''MYB'' gene region.]] | ||
| + | <br /> | ||
==Familial Forms== | ==Familial Forms== | ||
| − | + | <br /> | |
| − | |||
| − | |||
==Additional Information== | ==Additional Information== | ||
| − | + | <br /> | |
==Links== | ==Links== | ||
| − | + | <br /> | |
| − | == | + | ==Reference== |
<references /> | <references /> | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Notes== | ==Notes== | ||
<nowiki>*</nowiki>Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the CCGA coordinators (contact information provided on the homepage). Additional global feedback or concerns are also welcome. | <nowiki>*</nowiki>Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the CCGA coordinators (contact information provided on the homepage). Additional global feedback or concerns are also welcome. | ||
Latest revision as of 16:30, 12 July 2024
Primary Author(s)*
Katherine Geiersbach, MD, Mayo Clinic, and Jun Liao, PhD, Columbia University Irving Medical Center
Cancer Category/Type
Breast Cancer / Epithelial Tumours of the Breast
Cancer Sub-Classification / Subtype
Rare and Salivary Gland-type Tumours / Adenoid cystic carcinoma
Definition / Description of Disease
Invasive carcinoma with a characteristic histologic pattern, comprised of epithelial and myoepithelial cells. Epithelial cells form glands with lumina containing mucoid material; associated stromal matrix is present, forming irregular spaces called pseudolumina. Subtypes include classic adenoid cystic carcinoma, solid-basaloid adenoid cystic carcinoma, and adenoid cystic carcinoma with high-grade transformation.
Synonyms / Terminology
Cylindroma (Historical)
Epidemiology / Prevalence
Rare; approximately 0.1% of all breast cancers
Clinical Features
| Signs and Symptoms | Palpable breast mass, mainly in elderly patients
Suspicious lesion on mammography |
| Laboratory Findings | N/A |
Sites of Involvement
Any quadrant of the breast; retroareolar most common
Morphologic Features
Tubular, cribriform, and solid patterns are observed.
The classic subtype contains epithelial and myoepithelial cells with spaces called pseudolamina that contain stromal matrix with stromal cells (endothelial cells, fibroblasts) and basement membrane material (stains positive for collagen IV and laminin). Two cell populations are observed: an epithelial component that stains with low molecular weight cytokeratins (CK7, CK8), EMA, and sometimes CK5/6, and a myoepithelial component that stains with high molecular weight cytokeratins (CK14, CK5/6, p63) and typically also with myoepithelial markers (heavy-chain myosin, calponin, S100, CD10).
The solid basaloid subtype contains solid nests of basaloid cells with high grade nuclear features (marked nuclear atypia, high mitotic count, and necrosis).
Rare cases of adenoid cystic carcinoma can undergo high-grade transformation.
Immunophenotype
| Finding | Marker |
|---|---|
| Positive (universal) | Epithelial cells: low molecular weight cytokeratins CK7 and CK8; EMA; SOX10[1] |
| Positive (subset) | Epithelial cells: KIT (CD117)
Myoepithelial cells: heavy-chain myosin, calponin, S100, CD10, p63 |
| Negative (universal) | ER, PR, HER2, neuroendocrine markers (chromogranin, synaptophysin) |
| Negative (subset) |
Chromosomal Rearrangements (Gene Fusions)
Recurrent rearrangements of MYB (or, more rarely, the paralogous gene MYBL1) preserve the N-terminal DNA binding domain and transactivation domain in the chimeric gene product. The C-terminal regulatory domains of MYB or MYBL1 is generally absent in the active fusion, but the intact gene sequence is preserved in reported cases of MYB amplification and in some MYBL1 rearrangements.[3][4] Single cases of other fusions have been reported, including a KMT2C::WEE2 fusion reported by Schwartz and others[5],
| Chromosomal Rearrangement | Genes in Fusion (5’ or 3’ Segments) | Pathogenic Derivative | Prevalence | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|
| t(6;9)(q23.3;p23) | MYB::NFIB | der(6) | 54% | Yes | No | Yes | Most common fusion breakpoints involve exon 14 of MYB fused to exon 9 or exon 8c of NFIB.[3][6][7] |
| t(8;9)(q13.1;p23) | MYBL1::NFIB | Reported breakpoints involve exon 14 of MYBL1 fused to exon 9 of NFIB[4] | |||||
| t(6;v)(q23.3;v) | MYB | Fusions involving MYB with other gene partners or complex structural abnormalities associated with MYB gene fusion generate more complex karyotypes. Loss of 3' portion of MYB reported in one case[4]. Other reported MYB fusion partners include EWSR1 (with EWSR1 as the 5' partner, exon 10, fused to exon 2 of MYB)[8]. | |||||
| t(8;v)(q13.1;v) | MYBL1 | Fusions involving MYBL1 with other gene partners or more complex structural abnormalities associated with MYBL1 gene fusion generate more complex karyotypes. Other reported MYBL1 gene partners include ACTN1[4]. |
Individual Region Genomic Gain/Loss/LOH
Amplification or copy state transitions (gain or loss) on 6q23.3 associated with MYB rearrangement are the most commonly reported alterations in adenoid cystic carcinoma. Other individually reported alterations include gains of 1p36.12–p35.3, 11p15.5, 12p13.31, 16p13.3, and 19p13, and losses of 6q25.3-q26 and 9p11.1–q21.11 in an array CGH study of 14 adenoid cystic carcinomas by Wetterskog and others[9], gains of 17q21-q25.1 and losses of 12q12-q14.1 detected by whole exome sequencing on 12 adenoid cystic carcinoma in a study by Martelotto and others[7], and a terminal 6q loss in one case (6q23.3-6q27) and whole chromosome losses (-4, -7, -14, -X) in a second case by targeted next generation sequencing in a study by Fusco and others[10]. A terminal loss on 6q (6q23.3-6q27) detected by array CGH was separately reported in a case with MYB rearrangement by Kovacs and others[11]. Recurrent copy number alterations reported in a study by Masse and others included losses on 12q, losses or gains on 17p, and amplification of CCND1 on 11q13.3 detected by array CGH[12]. The common recurrent alterations are shown in the table below.
| Chr # | Gain / Loss / Amp / LOH | Minimal Region Genomic Coordinates [Genome Build] | Minimal Region Cytoband | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|
| 6 | Amp | chr6:135,502,453-135,540,311 [GRCh37/hg19] | 6q23.3 | Yes | No | No | MYB amplification in one case reported as a range of 3-10 copies by FISH associated with MYB overexpression[4]; two others reported in a study by Yao and others without copy number specified[13] |
| 6 | Gain or Loss | chr6:135,502,453-135,540,311 [GRCh37/hg19] | 6q23.3 | Yes | No | No | Copy state transitions within MYB gene region typically associated with MYB fusion[10][11] |
Characteristic Chromosomal Patterns
| Chromosomal Pattern | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|
| N/A | N/A | N/A | N/A | N/A |
Gene Mutations (SNV/INDEL)
Common recurrent mutations are shown in the table below. Others include ARID1A[12], PIK3R1[12], and TLN2[7].
| Gene; Genetic Alteration | Presumed Mechanism (Tumor Suppressor Gene [TSG] / Oncogene / Other) | Prevalence (COSMIC / TCGA / Other) | Concomitant Mutations | Mutually Exclusive Mutations | Diagnostic Significance (Yes, No or Unknown) | Prognostic Significance (Yes, No or Unknown) | Therapeutic Significance (Yes, No or Unknown) | Notes |
|---|---|---|---|---|---|---|---|---|
| NOTCH1, NOTCH2, and NOTCH3; sequence variants [12] | Gain of function | 22-28% solid basaloid subtype [5] [12] | Mostly solid basaloid subtype, with poorer prognosis [5] NOTCH mutations cause resistance to BET bromodomain inhibitors | |||||
| CREBBP; inactivating sequence variants [12] | Loss of function | 17-33% solid basaloid subtype [5][12] | Mostly solid basaloid subtype, with poorer prognosis | |||||
| KMT2C; inactivating sequence variants, deletion [12] | Loss of function | 22% solid basaloid subtype in one study [5] | Mostly solid basaloid subtype, with poorer prognosis | |||||
| KDM6A; inactivating sequence variants | Loss of function | 22% solid basaloid subtype in one study [5] | Mostly solid basaloid subtype, with poorer prognosis | |||||
| CDK12; missense[12] | Loss of function | 38% solid basaloid subtype in one study [12] | Mostly solid basaloid subtype, with poorer prognosis |
Note: A more extensive list of mutations can be found in cBioportal (https://www.cbioportal.org/), COSMIC (https://cancer.sanger.ac.uk/cosmic), ICGC (https://dcc.icgc.org/) and/or other databases.
Epigenomic Alterations
Genes and Main Pathways Involved
| Gene; Genetic Alteration | Pathway | Pathophysiologic Outcome |
|---|---|---|
| MYB; gene fusion or amplification | Cell cycle (MYC and NOTCH signaling), DNA replication, DNA repair | Promotes cellular proliferation |
| MYBL1; gene fusion | Cell cycle (MYC and NOTCH signaling), DNA replication, DNA repair | Promotes cellular proliferation |
| NOTCH1, NOTCH2, NOTCH3 | NOTCH signaling | Promotes cellular proliferation |
A study of adenoid cystic carcinoma of salivary glands by Drier and others delineates the mechanism of MYB gene pathway upregulation via rearrangements that increase MYB expression. MYB rearrangements typically juxtapose MYB with strong enhancers in regions downstream of NFIB, TGFBR3 and RAD51B. Gene fusions most often occur on the 3' side of MYB, a subset of gene fusions occur on the 5' side, and all serve to bring the MYB gene locus close to strong enhancer elements, thus upregulating MYB expression. The authors note that TP63 signaling is active in the myoepithelial component of low grade adenoid cystic carcinomas, while Notch signaling is active in luminal epithelial components. Furthermore, the authors suggest that Notch pathway mutations may underlie the switch to solid histology and the more aggressive clinical course of these tumors.[14]
Genetic Diagnostic Testing Methods
FISH for MYB rearrangement; RT-PCR for MYB-NFIB fusion transcript; RNA-based sequencing (whole transcriptome or targeted)
Familial Forms
Additional Information
Links
Reference
- ↑ 1.0 1.1 Yang, Chen; et al. (2019). "SOX10 Is a Sensitive Marker for Breast and Salivary Gland Adenoid Cystic Carcinoma: Immunohistochemical Characterization of Adenoid Cystic Carcinomas". Breast Cancer: Basic and Clinical Research. 13: 1178223419842185. doi:10.1177/1178223419842185. ISSN 1178-2234. PMC 6501487. PMID 31105427.
- ↑ Poling, Justin S.; et al. (2017-07). "MYB Labeling by Immunohistochemistry Is More Sensitive and Specific for Breast Adenoid Cystic Carcinoma than MYB Labeling by FISH". The American Journal of Surgical Pathology. 41 (7): 973–979. doi:10.1097/PAS.0000000000000878. ISSN 1532-0979. PMID 28498281. Check date values in:
|date=(help) - ↑ 3.0 3.1 Persson, Marta; et al. (2009-11-03). "Recurrent fusion of MYB and NFIB transcription factor genes in carcinomas of the breast and head and neck". Proceedings of the National Academy of Sciences of the United States of America. 106 (44): 18740–18744. doi:10.1073/pnas.0909114106. ISSN 1091-6490. PMC 2773970. PMID 19841262.
- ↑ 4.0 4.1 4.2 4.3 4.4 Kim, Jisun; et al. (2018-02). "MYBL1 rearrangements and MYB amplification in breast adenoid cystic carcinomas lacking the MYB-NFIB fusion gene". The Journal of Pathology. 244 (2): 143–150. doi:10.1002/path.5006. ISSN 1096-9896. PMC 5839480. PMID 29149504. Check date values in:
|date=(help) - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 Schwartz, Christopher J.; et al. (2022-02). "The clinical behavior and genomic features of the so-called adenoid cystic carcinomas of the solid variant with basaloid features". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 35 (2): 193–201. doi:10.1038/s41379-021-00931-6. ISSN 1530-0285. PMC 9197148 Check
|pmc=value (help). PMID 34599282 Check|pmid=value (help). Check date values in:|date=(help) - ↑ D'Alfonso, Timothy M.; et al. (2014-11). "MYB-NFIB gene fusion in adenoid cystic carcinoma of the breast with special focus paid to the solid variant with basaloid features". Human Pathology. 45 (11): 2270–2280. doi:10.1016/j.humpath.2014.07.013. ISSN 1532-8392. PMID 25217885. Check date values in:
|date=(help) - ↑ 7.0 7.1 7.2 Martelotto, Luciano G.; et al. (2015-10). "Genomic landscape of adenoid cystic carcinoma of the breast". The Journal of Pathology. 237 (2): 179–189. doi:10.1002/path.4573. ISSN 1096-9896. PMC 4676955. PMID 26095796. Check date values in:
|date=(help) - ↑ Lei, Ting; et al. (2023-01-31). "A novel EWSR1-MYB fusion in an aggressive advanced breast adenoid cystic carcinoma with mixed classical and solid-basaloid components". Virchows Archiv: An International Journal of Pathology. doi:10.1007/s00428-023-03500-1. ISSN 1432-2307. PMID 36719454 Check
|pmid=value (help). - ↑ Wetterskog, Daniel; et al. (2012-01). "Adenoid cystic carcinomas constitute a genomically distinct subgroup of triple-negative and basal-like breast cancers". The Journal of Pathology. 226 (1): 84–96. doi:10.1002/path.2974. ISSN 1096-9896. PMID 22015727. Check date values in:
|date=(help) - ↑ 10.0 10.1 Fusco, Nicola; et al. (2016-11). "Genetic events in the progression of adenoid cystic carcinoma of the breast to high-grade triple-negative breast cancer". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 29 (11): 1292–1305. doi:10.1038/modpathol.2016.134. ISSN 1530-0285. PMC 5083185. PMID 27491809. Check date values in:
|date=(help) - ↑ 11.0 11.1 Kovács, Anikó; et al. (2017-09). "Genomic imbalances and MYB fusion in synchronous bilateral adenoid cystic carcinoma and invasive lobular carcinoma of the breast". Molecular and Clinical Oncology. 7 (3): 322–326. doi:10.3892/mco.2017.1330. ISSN 2049-9450. PMC 5582535. PMID 28894575. Check date values in:
|date=(help) - ↑ 12.0 12.1 12.2 12.3 12.4 12.5 12.6 12.7 12.8 12.9 Massé, Julie; et al. (2020-06). "Solid-type adenoid cystic carcinoma of the breast, a distinct molecular entity enriched in NOTCH and CREBBP mutations". Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc. 33 (6): 1041–1055. doi:10.1038/s41379-019-0425-3. ISSN 1530-0285. PMID 31857685. Check date values in:
|date=(help) - ↑ Yao, Qian; et al. (2022). "Comparative proteomic and clinicopathological analysis of breast adenoid cystic carcinoma and basal-like triple-negative breast cancer". Frontiers in Medicine. 9: 943887. doi:10.3389/fmed.2022.943887. ISSN 2296-858X. PMC 9366086 Check
|pmc=value (help). PMID 35966872 Check|pmid=value (help). - ↑ Drier, Yotam; et al. (2016-03). "An oncogenic MYB feedback loop drives alternate cell fates in adenoid cystic carcinoma". Nature Genetics. 48 (3): 265–272. doi:10.1038/ng.3502. ISSN 1546-1718. PMC 4767593. PMID 26829750. Check date values in:
|date=(help)
Notes
*Primary authors will typically be those that initially create and complete the content of a page. If a subsequent user modifies the content and feels the effort put forth is of high enough significance to warrant listing in the authorship section, please contact the CCGA coordinators (contact information provided on the homepage). Additional global feedback or concerns are also welcome.